Periodontal bone augmentation procedures often require coverage of the graft material with barrier membranes to protect the regenerating tissues, isolate them from environmental factors, and enable healing. Along with bone graft materials, barrier membranes play an important role in regenerating lost periodontal and peri-implant tissues. This article discusses dental barrier membranes and bone graft substitutes used in periodontal regenerative procedures.
Types of Dental Barrier Membranes
There are different types of barrier membranes based on their origin and composition:
Non-resorbable membranes:
Made from non-bioresorbable materials like titanium, Teflon, polytetrafluoroethylene (PTFE), they can remain for longer durations in the body. However, they require removal surgery after a few months.
Bioabsorbable/Resorbable membranes:
Further classified as:
Collagen membranes: Derived from animal sources like bovine, porcine collagen or human collagen. They get resorbed within 4-6 weeks by enzymatic degradation. Examples include Bio-Gide, Ossix Plus.
Synthetic bioabsorbable membranes: Made from polylactic acid (PLA) and polyglycolic acid (PGA). Examples are LactoSorb and Vicryl. They degrade by hydrolysis and get resorbed within 2-6 months.
Allograft-derived membranes: Obtained from processed human tissues like dermis matrix, amnion/chorion membrane. Examples are AlloDerm, AlloMax.
Xenograft-derived membranes: Derived from processed animal tissues like porcine or bovine pericardium. Examples are BioMend and Geistlich Bio-Gide.
The choice depends on clinical situation, membrane properties, resorption time and patient’s own healing response. Resorbable membranes are preferred to avoid secondary surgery for membrane removal.
Bone Graft Substitute Materials
A variety of bone graft materials are available as substitutes to autografts for periodontal and peri-implant ridge augmentation:
Allografts: Demineralized freeze-dried bone allograft (DFDBA) or mineralized freeze-dried bone allograft (FDBA) obtained from human cadavers. Examples are Grafton DBM and OsteoGraf.
Xenografts: Bovine-derived mineralized bone chips like Bio-Oss. Shown to be biocompatible and osteoconductive.
Alloplasts: Synthetic bone substitutes like hydroxyapatite (HA) and beta-tricalcium phosphate (β-TCP). They are osteoconductive and get incorporated into new bone. Examples include OsteoGraf R and Cerabone.
Bone morphogenetic proteins (BMPs): BMP-2 and BMP-7 promote osteogenesis. Example is Infuse. Used with a collagen sponge carrier.
Demineralized bone matrix (DBM): Obtained by acid extraction of allograft cancellous bone chips retaining osteoinductive growth factors. Examples are Grafton DBM Plus and OsteoBiologics DBX.
Their osteoconductivity and osteoinductivity depends on type, preparation method and carrier used. Combining different graft materials may enhance regenerative outcomes.
Periodontal Regeneration Process Using Membranes and Grafts
During periodontal regeneration procedures, after thorough debridement and surface conditioning, the defects are filled with bone graft substitutes.
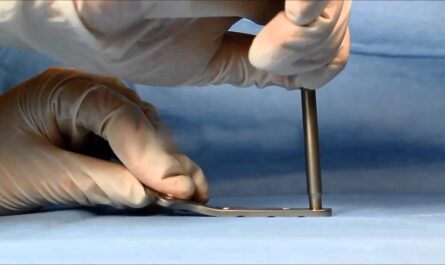
A resorbable membrane is trimmed and adapted to cover the grafted area, extending few millimeters beyond bone edges on all aspects to enable guided tissue regeneration (GTR). Sutures are placed to stabilize the membrane.
Over next 4-6 weeks, the barrier membrane allows migration and proliferation of periodontal ligament cells and osteoblasts underneath while excluding gingival connective tissue cell migration.
Osteoinductive factors in bone grafts trigger differentiation of progenitor cells to osteoblasts. New cementum, periodontal ligament and alveolar bone are regenerated in place of the lost tissues, restoring periodontal function and support.
The outcomes majorly depend on defect morphology, membrane seal, patient’s bacterial control and healing ability. Post-operative care includes antibiotics and follow-up.
Complications and Latest Advancements
Infections, membrane exposure, graft washout due to poor seal are challenges. Success rate is nearly 80% for intra-bony defects and 70% for furcation involvement.
Latest technologies include use of biocompatible synthetic membranes instead of animal derivatives to reduce immunogenicity risks.
Resorbable meshes for precise space maintenance of customized grafts are gaining popularity over solid block grafts.
Tissue-engineered bone grafts using patients’ own cells on 3D scaffolds provide better control over revascularization and bone formation.
Computer-guided regenerative procedures using CBCT-based templates and custom implant placement improve predictability and outcomes.
Gene, growth factor and stem cell therapies may help regenerate larger defects in future by precisely controlling cell differentiation pathways.
Overall, dental membranes and bone graft substitutes significantly enhance the predictability of periodontal regeneration when used judiciously along with standard surgical and hygiene protocols. Outcomes continue improving with advancements in material sciences and tissue engineering approaches.
Conclusion
The article provided an overview of commonly used dental barrier membranes and bone graft substitutes in periodontal regenerative procedures. It discussed their types, role in regeneration process and briefly touched upon latest technological developments. With advancements enhancing effectiveness and controlling challenges better, periodontal regeneration is becoming a more predictable treatment modality for restoring lost periodontal support.
*Note:
1. Source: Coherent Market Insights, Public sources, Desk research
2. We have leveraged AI tools to mine information and compile it