Pulmonary edema, or fluid buildup in the lungs, is a serious medical condition characterized by impaired gas exchange. It occurs when fluid leaks from blood vessels into the air sacs of the lungs due to increased pressure in the capillaries that line the lungs. Left untreated, pulmonary edema can lead to hypoxemia, organ damage, and even death. In this article, we explore the various therapeutic options currently available to treat pulmonary edema as well as some emerging treatments under investigation.
Pathophysiology and Diagnosis
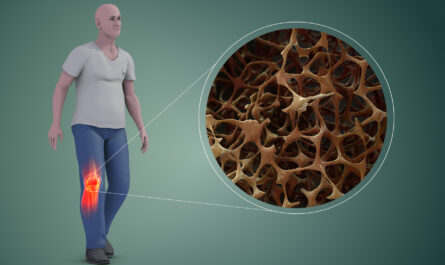
Pulmonary edema occurs when the pressure in the pulmonary capillaries rises above that in the left atrium of the heart, causing fluid to leak from blood vessels into lung tissue. The main causes of this elevated capillary pressure include left ventricular failure, inflammation of the lungs ( pneumonia), acute respiratory distress syndrome (ARDS), kidney failure, and severe burns or trauma. Pulmonary edema is diagnosed based on symptoms like shortness of breath, coughing, chest pain or tightness, and pink, frothy sputum. Chest x-rays and analysis of fluids obtained via bronchoscopy may also help confirm the presence of excess lung fluids.
Conventional Drug Therapies
The first-line treatment for acute Pulmonary Edema Therapeutics involves supplemental oxygen therapy, diuretics like furosemide to remove excess fluids from tissues and lungs, and therapies aimed at addressing the underlying cause like antibiotics for pneumonia. Vasodilators like nitroglycerin may also be used to lower blood pressure in the lungs, thereby reducing fluid leakage into lung tissues. Additionally, positive airway pressure from methods like continuous positive airway pressure (CPAP) and bilevel positive airway pressure (BiPAP) helps reduce workload on the heart and lungs while improving oxygen delivery. For severe cases refractory to initial therapy, more invasive procedures like intubation and mechanical ventilation may be required.
Emerging Pharmacological Treatments
While diuretics and vasodilators remain mainstay therapies, new drugs are being investigated for pulmonary edema:
– Nitric Oxide: Inhaled nitric oxide is a selective pulmonary vasodilator that improves blood oxygenation, by selectively lowering pressures in the pulmonary circulation. It is under study for treatment of acute respiratory distress syndrome (ARDS).
– Statins: Statins have pleiotropic effects beyond cholesterol-lowering. Studies show their potential to reduce endothelial permeability, inflammation, and pulmonary vascular remodeling in animal models of lung injury. They may offer new adjuvant therapies for pulmonary edema and ARDS.
– Angiotensin-Converting Enzyme (ACE) Inhibitors: ACE inhibitors block the conversion of angiotensin I to the potent vasoconstrictor angiotensin II. They reduce pulmonary arterial pressure and promote resorption of lung fluids. However, human trials are still needed to establish their role as adjuvant therapies.
– Stem Cell Therapies: Mesenchymal stem cells secrete paracrine mediators with reparative and anti-inflammatory properties. Preclinical studies indicate their potential therapeutic benefit for pulmonary fibrosis, ARDS, and lung injury resolution. Phase I trials are ongoing for use in ARDS patients.
Non-Pharmacological Treatment
Beyond medications, other non-drug therapies help manage pulmonary edema:
– Diuresis: The withdrawal of excessive fluids from circulation via intravenous furosemide reduces hydrostatic pressures and fluid overload in lungs and tissues. Monitoring of renal function is important during diuresis.
– Oxygen Therapy: Supplemental oxygen increases the driving pressure for diffusion of oxygen into tissues, improving hypoxemia. It is delivered via nasal cannula, mask, CPAP/BiPAP, or mechanical ventilation based on severity.
– Ventilation Support: Noninvasive ventilation via CPAP/BiPAP reduces work of breathing and promotes lung recruitment. For severe cases, endotracheal intubation and mechanical ventilation are life-saving by fully taking over ventilation.
– Lung Recruitment Maneuvers: Strategies like sustained inflation breath-holds and increased PEEP usage recruit collapsed lung units and improve ventilation-perfusion mismatching. They help resolve pulmonary edema when used judiciously.
– Hemodynamic Monitoring: Pulmonary artery catheters assess cardiac filling pressures, which guide diuretic therapy and optimization of preload and afterload in cardiac edema. Other advanced monitoring with echocardiography also aids management.
– Renal Replacement Therapy: For patients with acute kidney injury and fluid overload refractory to diuretics, renal replacement therapy via continuous venovenous hemofiltration promotes fluid removal and correction of electrolyte and acid-base disturbances.
Outcomes and Prognosis
With appropriate treatment guided by careful monitoring and addressing of underlying causes, prognosis is good for most cases of pulmonary edema. Improvement in symptoms and lung images is seen within hours to days with therapy. However, patients with pre-existing cardiac dysfunction or those developing complications like ARDS have worse outcomes. Ongoing research into new drugs and technologies is needed to further enhance the management and survival in severe cases of pulmonary edema.
*Note:
1. Source: Coherent Market Insights, Public sources, Desk research
2. We have leveraged AI tools to mine information and compile it