Introduction to cancer biologics
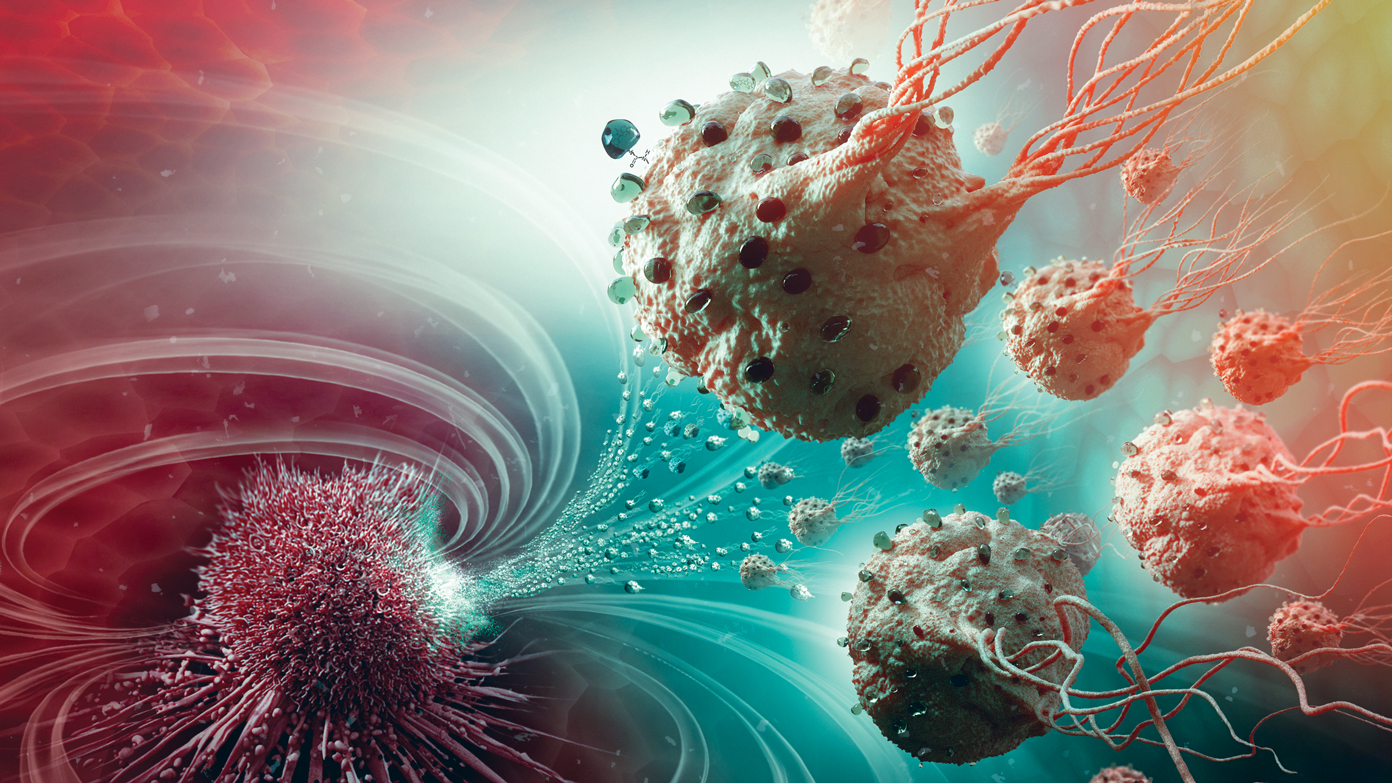
Cancer biologics, also known as biological therapies or biological response modifiers, utilize the body’s immune system or natural substances occurring in the body to fight cancer. They are designed to either boost the body’s natural defenses against cancer or to directly target specific proteins on cancer cells to limit their growth and survival. Some key types of cancer biologics include monoclonal antibodies, vaccines, checkpoint inhibitors, and cytokine treatments.
Monoclonal antibodies as targeted cancer therapies
Monoclonal antibodies (mAbs) are synthetic versions of immune system proteins that are designed to bind to specific targets on cancer cells. This binding helps to recognize cancer cells as foreign so they can be destroyed by the immune system. Some examples of monoclonal antibodies used in cancer treatment include trastuzumab (Herceptin) for HER2-positive breast cancer, rituximab (Rituxan) for lymphoma, and bevacizumab (Avastin) which inhibits the growth of new blood vessels that tumors need to grow. mAbs can also directly induce cancer cell death or activate the immune system to attack cancer cells. They are tailored to recognize epitopes, or molecular features, that are specific to tumor cells. This precision targeting allows mAbs to destroy cancer cells while sparing healthy tissues.
Adoptive cell transfer using T-cells
Adoptive cell transfer (ACT) is an emerging cancer immunotherapy approach that utilizes T-cells, a type of white blood cell critical to the immune response. In ACT, T-cells are removed from a cancer patient and genetically engineered to more effectively recognize and attack cancer cells. The modified T-cells are then grown in large numbers in the laboratory and infused back into the patient to target cancer. This type of therapy harnesses the power of a patient’s own immune system to seek out and destroy tumors from within. ACT holds promise for treating certain blood cancers as well as solid tumors like melanoma, lung cancer, and others. Ongoing research continues to develop methods for targeting a wider range of cancers using T-cell therapies.
Cancer vaccines to stimulate anti-tumor immunity
Cancer vaccines aim to boost the body’s natural defenses against cancer by activating the immune system through antigen presentation. They work by exposing the immune system to antigens, typically proteins, from cancer cells without actually injecting Cancer Biologics cells. This primes the immune system to recognize those antigens as foreign and gives rise to a cascade of immune cells that can then seek out and destroy tumor cells expressing those antigens. Different types of cancer vaccines include preventative, therapeutic, and personalized vaccines. Sipuleucel-T was the first therapeutic cancer vaccine approved by the FDA for treatment of prostate cancer. It utilizes autologous dendritic cells primed with a prostate antigen to trigger an anti-tumor immune response. Research continues on developing more effective vaccines against various malignancies.
Checkpoint inhibitors release brakes on immune response
Cancer cells have developed mechanisms to evade detection and destruction by the immune system. Key pathways known as immune checkpoints act as brakes that stop T-cells from attacking cancer cells. Checkpoint inhibitors are a class of immunotherapies that target these pathways to “release the brakes” and unleash a potent anti-tumor response. For example, CTLA-4 checkpoint inhibitors like ipilimumab block the CTLA-4 receptor to enhance T-cell proliferation and activate immune cells. PD-1 inhibitors including nivolumab and pembrolizumab work similarly by blocking the PD-1 pathway utilized by cancer cells to inhibit T-cell activity. Checkpoint inhibitors have demonstrated durable responses across many cancer types like melanoma, lung cancer, and more. They work synergistically with other immunotherapies to boost anti-tumor immunity.
Cytokines support immune system rebuilding and activation
Cytokines are endogenous Cancer Biologics proteins that regulate maturation, growth, and responsiveness of immune cells. Certain cytokines like interferons, interleukins, and colony-stimulating factors play important roles in cancer immunotherapies by augmenting various aspects of the immune response against tumors. For example, interferon-alpha is used to treat some forms of leukemia as well as melanoma and renal cell carcinoma. It has anti-proliferative and immunomodulatory properties. Interleukin-2 stimulates T-cell and NK cell proliferation and is FDA-approved for treatment of melanoma and renal cell carcinoma. GM-CSF helps stimulate stem cell proliferation and differentiation into granulocytes and monocytes. It can repair damaged immune systems during cancer treatment with chemotherapy or radiation. Carefully administered cytokines can help strengthen and activate the immune response against malignancies.
Toxicities and management of immune related adverse events
While promising, immunotherapies may also cause immune related adverse events (irAEs) as a result of overactive or misdirected immune system activation against normal tissues. Common irAEs include skin rashes, colitis, hepatitis, hypophysitis, and pneumonitis. These side effects are usually mild to moderate but can sometimes be life-threatening. Careful screening, early detection, and prompt immunosuppressive treatment with corticosteroids are important aspects of managing irAEs. Combination immunotherapies may pose greater risk of side effects than single agents. However, irAEs are often manageable with proper protocol. The long term benefits of immuno-oncologic agents continue to outweigh associated risks for many patients with refractory cancers. Ongoing research also aims to minimize treatment-related harm.
*Note:
1. Source: Coherent Market Insights, Public sources, Desk research
2. We have leveraged AI tools to mine information and compile it.